Centers for Independent Living (CILs) and other community-based organizations (CBOs) have a prime opportunity to develop new contracts with health care providers and payers, including health plans, as these organizations seek to engage with CBOs for their expertise in improving services to and outcomes of clients. The roots that CILs have in consumer direction can be an asset and value to partners and those they serve. The time is now to get involved in this new arena—developing new payers can drive revenues to your agency and help ensure that the consumers you serve receive a full scope of services.
If you are just beginning on this path, it can be difficult to know where to start. In working with the Aging and Disability Business Institute, ILRU and the National Center for Aging and Disability have developed a How-To Guide for Marketing Centers for Independent Living Services to Health Plans and Payers. Much of the information in this guide is drawn from the experiences of other CILs and Area Agencies on Aging (AAA) who have successfully embarked on this journey. Many have negotiated contracts in the areas of case management, care transitions, home care, nutrition programs, person-centered planning, participant-directed care and transportation. Though there’s no one-size-fits-all approach, this guide will lead you through a variety of steps necessary to begin and move forward in this work.
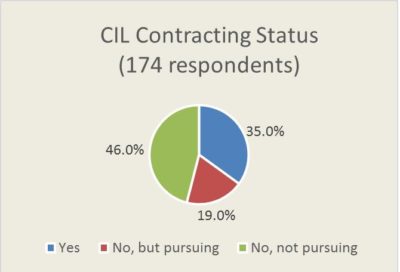
In 2017 and 2018, the Aging and Disability Business Institute partnered with Scripps Gerontology Center to collect responses from CILs, AAAs and other community-based organizations to learn about their health care contracting work. The resulting report, Community-Based Organizations and Health Care Contracting: Building & Strengthening Partnerships, shows that more than half—54 percent—of the CIL respondents had or were pursuing a contract, up from 45.4 percent in the prior year.
CILs’ strong philosophy of consumer direction and regular interaction with people with disabilities brings an enormous value to working with health plans. What are the needs in your community? What is your niche? Health plans and other payers need your expertise but often do not know anything about your agency so you’ll have to educate and make a strong value proposition for your services. Some potential payers in your community include:
- Medicaid Managed Care Organizations
- Accountable Care Organizations
- Hospital or Health Systems
- Veterans Administration (VA) Medical Centers
- Duals Plans
- State Medicaid Agencies
- Commercial Health Insurance Plans
Do these potential partners know who you are and what you do? Educating and marketing your services to health plans and payers provides an opportunity to introduce yourself and share your strengths. Demonstrate your value by bringing a one-page overview describing the populations you serve and the services and programs you provide. Building a personal relationship is important, and listening to the payer’s potential needs is a critical piece to define. Now, where can you support or fill in the gaps?
This new guide provides resources and tips from experts in the field as you plan to expand your reach with new health care entities. It is full of linked resources when you are ready to dive deeper into the process. No matter what size your organization is, if you serve a rural or urban population, there are opportunities to grow in this new arena. These partnerships are growing and reimbursement methodologies are changing—it’s time to get involved.
For a more detailed breakdown watch our December 6, 2018, introductory webinar. Also, be sure to check out the full guide on our resource page.